There is some serious mathematics and epidemiology that underpins this. I will link to some of the publications at the end. However what I hope to do here is show the principle and how it intuitively makes sense that small time differences in actions have very large effects. This is because epidemics like this (with a very highly infectious disease) grow exponentially. This is very much a back-of-an-envelope type of calculation but the charts make the concept clear and the estimates that I end up with are completely in line with (although not as precise as) those generated by using formal complex modeling.
Here's a very silly example. If you place 1p on the first square of a chess board and then 2p on the next, 4p on the third and 8p on the fourth, then 16p, then 32p, then 64p and £1.28 on the last one of that row; your first row only adds up to £2.55. But if you keep going like that the total value you end up with at the 64th square is an astounding One hundred and eighty thousand, trillion pounds! Obviously, the biggest problem with this thought experiment is that you very quickly run out of physical space on each square of the board. Exponential growth is difficult to imagine but quite easy to model mathematically.
We see exponential growth in epidemics because generally speaking, each person who gets infected, infects in-turn, two or three or more other people. And thus the total number of people affected doubles and doubles and doubles again very quickly.
At the height of the pandemic, official estimates had UK case numbers doubling every 2 days.
So, let us have a look at the UK death figures.
There's a few things to consider here. Firstly the most reliable estimate of deaths from Covid-19 are the excess death figures. However, the best day-to-day dataset is the in-hospital deaths in people who tested positive for Covid-19. In the next paragraph I will explain the differences between these data and the importance of each. However, the short version is that for this calculation and demonstration I will use the hospital-deaths in England figures. The fact that these are incomplete does not matter for this example as it's all about the proportions. What we do need though is day-to-day tallys in order to do the calculations and thus these data are best for this.These day-to-day totals track the pandemic. The death figures are approximately two weeks behind the infection rates (which were not measured accurately at this point).
With Covid-19 there are three categories of mortality to consider. Covid-19 kills (primarily) vulnerable people. By-definition, vulnerable people have a high mortality anyway. That's what vulnerable means. If you take the entire population of the UK that is over 80 years old, approximately 15% of them will die in the next twelve months (without a Covid pandemic). For those aged 20-29 the same figure would be less than 1%. If someone has heart-failure and contracts Covid-19 then they are quite likely to die from it. However, they are quite likely to die anyway. So, in one-sense the Covid-19 is purely the terminal event and it would be more precise perhaps to attribute the death to heart failure. On the individual level it is impossible to untangle these things but on a population level, it is possible to see these effects. If we go back to our over-80s population then only 85% would be expected to be alive in 12 months' time. If Covid hitting this population means that when we look a year later only 55% are still alive then we could easily argue that 15% would have died anyway, but 30% wouldn't. Thus we could infer that 2/3rds of the deaths (30% out of 45%) were due to Covid. This is important because in the real world some people die from Covid-19 without being tested. Conversely some people who test positive for Covid-19 actually died from something else. And sometimes it's really hard to tell. There is also another thing to consider and that is the knock-on-effects of the pandemic. People presented less to hospital because they were worried about the risk of contracting Covid-19 in hospital (an appropriate fear) and thus it is likely that deaths from heart attacks and strokes may have been higher than normal. Not to mention delays in cancer care etc. It is correct to attribute these deaths to the pandemic because it is the effect of the disease on society that causes these changes in behaviour. Similarly, it would not be surprising if the extreme stretch in hospital resources meant that care was not quite as good as normal. Again on the individual level it would be difficult to unravel this but a spike in other causes of death would reflect this. What I mean is, if you take 100 people who have a heart attack, normally you would expect 75 of them to survive. If you found that during Covid times only 70 out of 100 survived that is a measurable effect but on the individual level it would be very difficult to precisely determine which of the thirty deaths would have happened anyway (25) and which of them would have survived in normal times(5). So the three categories are:
- Those that would have died in a 3-6 month period but Covid-19 was the terminal event
- Those that had a normal life expectency but died directly from Covid-19
- Those who died from some other cause but would not have done so in non-pandemic times.
There is a fourth category that has the opposite effect on total mortality. That is that reduced activity (particularly the massive drop in traffic numbers) probably resulted in a reduced death rate from road-traffic accidents directly and asthma (and other respiratory diseases) indirectly due to improved air quality.
The bottom line here is that the only way to understand the total number of deaths due to the Covid-19 pandemic is to look at the excess mortality over the whole time period. In the UK excess mortality is simply calculated by looking at the average death rates over 5 years (for the week/month/whole year) and comparing that with the same time period in 2020. (Different countries calculate this by slightly different methods but the principle is the same).
The major strength of this approach is that it will encapsulate all of the categories I've described and will also capture the large numbers who died from Covid-19 without being tested. However, excess mortality can only be done retrospectively and is entirely useless for tracking the progress of the pandemic and thus determining the effect of the lockdown. However with the daily death totals we can estimate the effect of lockdowns as a proportion of total deaths and thus apply that to the excess mortality figures to estimate how many deaths might have been prevented by an earlier lockdown.
I just want to pause here and note that each excess death is a real person and real tragedy for them and their loved ones. The question is to what extent some of these deaths might have been avoided.
This is the NHS England official daily deaths, available from here (data used covers up to 14th September):

The grey box indicates the time from initiation of lockdown to the peak of death rates. This delay reflects the incubation period of the virus and the clinical progress from displaying symptoms to death. This time-frame will vary between patients but overall will average out the same. Thus we can estimate what the curve would look like if we move the time point at which lockdown is introduced.
For example, this is what the chart looks like if we hadn't locked down on 23rd March but waited a week:
The principle here is that the number of people infected (and thus the number of deaths which is a proportion of this) will keep on growing until something changes. That 'something' could be that there are no-more people left in the population who are susceptible to the virus or it could be that people's behaviour changes profoundly and thus infection rates drop off. The former would happen eventually but even at the peak of the infection, probably the number of people infected was measured in the hundreds of thousands out of a population of 60 million. Thus there was still plenty more people for the virus to infect. Thus, in this example, the infection rate carries on growing exponentially for a further week, and therefore the peak is later by a week and much higher. In this model, the total death toll is more than doubled. If there was no government intervention (and no effective treatment etc.) eventually the death rate will plateau as the number of susceptible people in the population falls (as those left have been exposed to the virus and not become ill) or because people's behaviour has dramatically changed anyway. This is what happened with bubonic plague - civil society broke down and thus people stopped mingling and eventually the plagues died out.Conversely, intervening with shutdown earlier has profound positive effects:
If Lockdown had been introduced a week earlier then the peak would only have been ~650 deaths/day and ~250/day if it had been two weeks. What this adds up to is a 55% reduction or and 80% reduction in the total death-toll.
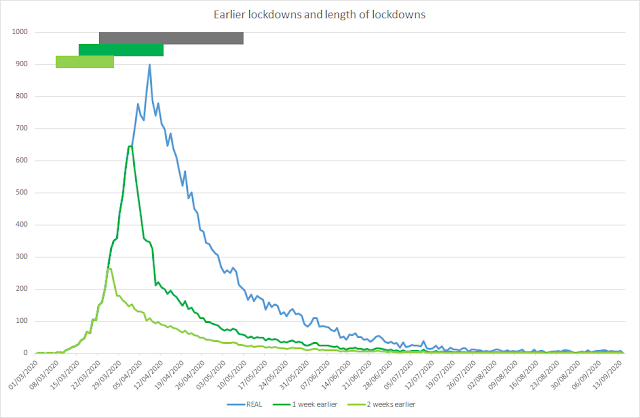
Our final chart highlights that earlier lockdowns also mean shorted lockdowns. If we assume the easing of some restrictions on 10th May was appropriate - i.e.the circulating levels of the virus was low enough to make this safe then we can estimate when the same level would have been achieved with the potential earlier lockdowns.
The grey box indicates the real Lockdown that happened (23rd March to 10th May). The green boxes represent the Lockdown times that would have been needed to achieve the same low level of new cases. Note how these time periods are significantly shorter.
I just want to reiterate here that these charts are produced by a very quick-and-dirty method but I hope they show intuitively why when you have a death rate growing exponentially, small differences in timing of actions have very large effects. This is particularly obvious in the last chart. Having said that, the figures I have produced by this are in line with the estimates produced by sophisticated modeling by epidemiologists and mathematicians who are expert at this. Therefore I feel confident that these charts are a good approximation and demonstrate the concepts very well.
So the conclusion of this is that locking down a week earlier results in 55% less deaths and two weeks, 80%. These are estimates and if we calculated the confidence intervals they would be wide but let's take those estimates and apply them to the excess mortality data described earlier.
This is a recent publication in the British Medical Journal which examines excess death rates. Using a similar method the Financial Times puts the UK death-toll (based on excess mortality) at 65,700 (upto 11th September 2020). By combining these two sets of data we can postulate that introducing the lockdown a week earlier would have led to 36,000 fewer deaths and if we'd done it two weeks earlier, 52,000 fewer.
As I said, this is a crude methodology and those figures are not precise estimates. However it is still accurate to say that locking down, even 1 week earlier would have meant tens of thousands fewer deaths as well as a much smaller economic cost as the lockdown would also have been shorter.